Trigger Warning: The following contains mention of sensitive subjects such as difficult nightmares and thoughts of suicide that may be triggering to some audiences.
In the 11 years I’ve been seeking help for my mental health conditions of depression, anxiety, borderline personality disorder (BPD) and complex-PTSD, I have been in and out of dozens of therapists’ offices and on hundreds of different medication prescriptions. I have meticulously followed every recommendation from every professional (several times to my detriment), and yet I have not experienced significant reduction of my symptoms. External life events indicate outwardly-facing successes: three amazing kids, college degree, university degree, my own photography business and blog, a job I love. Yet, through all of these events, I was inwardly experiencing so much suffering that, many times, I have so desperately wanted the pain to end that I wanted my life to end.
The world, the government, medical and religious communities, and even friends and family, seem to have compassion for external pain and physical disabilities, bringing financial resources and “casseroles,” which I applaud. In my experience, the great majority of these same circles turn their backs on emotional pain in a way that is beyond comprehension. In the general world, I have to “feel my way” around a person to see if they are safe to talk to. There are no government resources for my emotional disability since I am considered to be “high functioning,” and there is obscenely little government-funded medical research on the borderline brain to discover pharmacological and/or other medical treatments.
BPD is a health condition recognized in the Diagnostic Statistics Manual. Doctors are to use it to diagnose and treat medical conditions. Yet, an emergency room doctor once told me, “Well, you can’t expect me to know anything about borderline personality disorder!” And, why is that? Ten percent of us die by suicide! Maybe I’m missing something. There’s a new trend to say, “Mental health care IS health care,” but I say, “Why is, or, why has there ever been, a differentiation? My brain is not working the way it works in people without these conditions; since when was my brain not a part of my body!?!”
Research has established that there is “something” (we don’t yet know what) different with the way the logical side of my brain (my cortex), is or is not connecting to the very intense “fight or flight” part of my brain (my amygdala). Yet, psychiatrists often don’t correctly diagnose it, and medical insurance usually does not cover standard treatment which has shown over 20 years of research establishing it as being the most effective treatment for those struggling with suicidal thoughts and behaviors. I’m pretty sure, if there were new forms of cancer which had an evidence-based pharmacological or surgical treatment, 20 years would not go by before that treatment was used and covered in some substantial way by insurance, even though there wasn’t enough research to say why the person had that form of cancer.
My whole life I have believed untruths about myself and have repressed memories of childhood abuse (i.e. I avoided talking or even thinking about them) to the point of creating problems with my memory, especially of my more traumatizing experiences. In early 2020, I began experiencing horribly frightening nightmares where someone is trying to kill me or torture me. I would wake up yelling, “Don’t kill me! Stop! Don’t hurt me!” Most mornings I wake up terrified, full of dread of facing another day of pain.
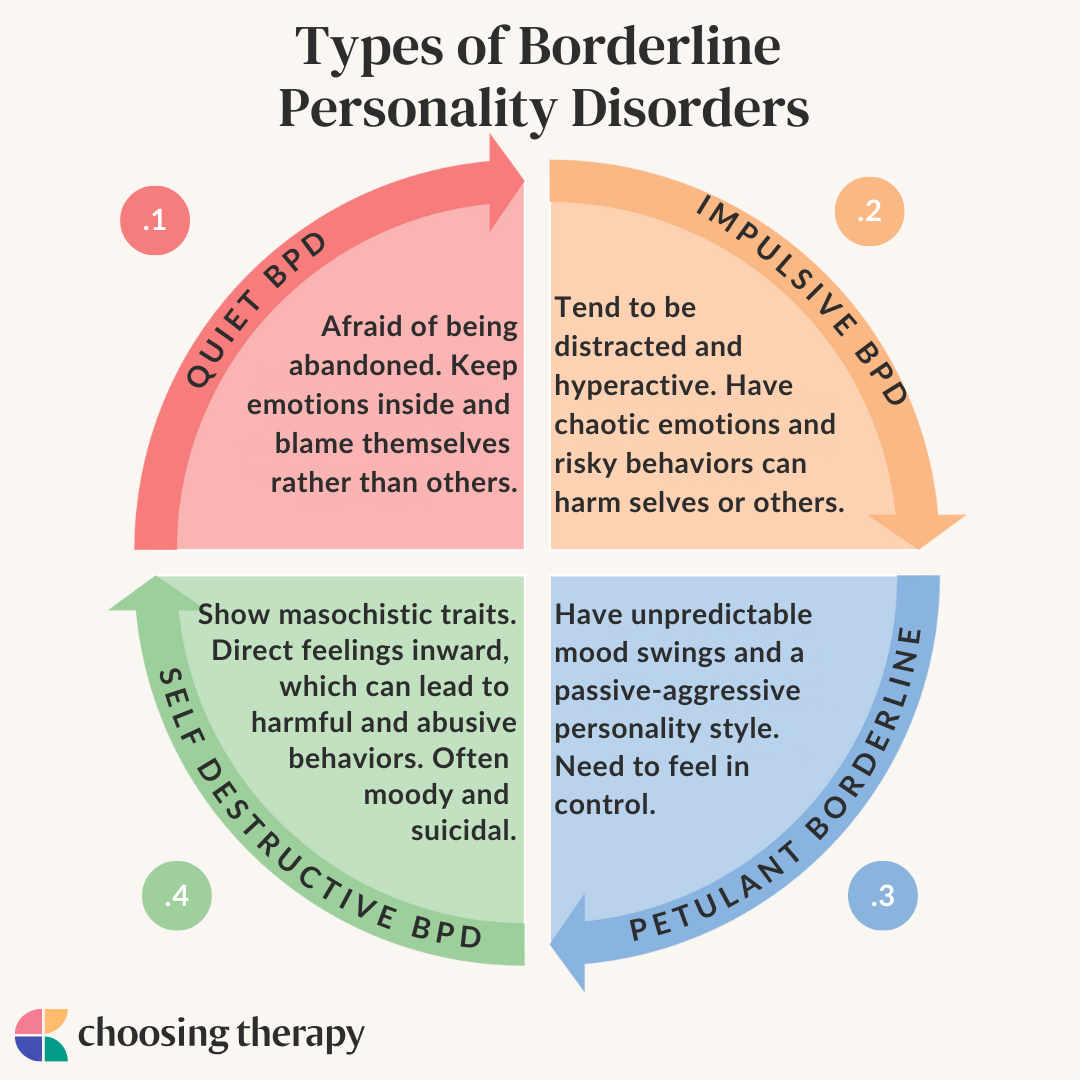
But, what exactly is BPD (Borderline Personality Disorder)?
BPD doesn't occur alone...
Effective treatment involves addressing related disorders.
Many people diagnosed with borderline personality disorder experience other conditions, including:
- Depression
- Anxiety disorders
- Eating disorders
- Post-traumatic stress disorder (PTSD)
- Bipolar disorder
- Substance use disorder
This disorder is misunderstood by many, including some mental health practitioners. This confusion can impact and influence the way that people are treated.
Even worse, long-standing myths can discourage people from seeking help for the condition, especially if they feel their experience is being misunderstood.
Myth: BPD Does Not Occur in People Younger Than 18
This remains one of the most persistent myths and misconceptions about BPD. Neither the current Diagnostic and Statistical Manual of Mental Disorders (DSM) nor the older versions of the DSM prohibit the diagnosis of BPD in people younger than 18.
According to McLean’s Blaise Aguirre, MD, “It is outrageous to think a clinician would not diagnose BPD when a person is seventeen years and 364 days old and then diagnose it the next day when the teen turns eighteen.” The sooner the diagnosis is made, the sooner treatment can begin.
Myth: BPD Is a Rare Condition
BPD is not a rare condition. Many people have heard of schizophrenia, which occurs in less than 1% of U.S. adults, and BPD is even more common.
Borderline personality disorder affects an estimated 1.4% of U.S. adults. This number may be higher, however, because many people with BPD are misdiagnosed with PTSD, ADHD, bipolar disorder, or depression.
An estimated 10% of psychiatric outpatients, 20% of psychiatric inpatients, and 6% of people visiting their primary health care provider have BPD.
Myth: BPD Is Not Treatable
Borderline personality disorder is very treatable. In the past, since BPD affects someone’s personality, many were quick to conclude that it was untreatable because someone’s personality cannot be changed.
More recently, many therapies have been proven effective as treatments, including dialectical behavior therapy (DBT), mentalization-based treatment (MBT), and transference-focused psychotherapy (TFP).
Now, a growing number of less intensive, generalist approaches, like general psychiatric management (GPM), are also being practiced around the world.
A BPD diagnosis doesn’t mean that someone will live with symptoms forever. With treatment, the symptoms ebb and flow. Many people with the condition can have high-functioning lives.
Myth: People With BPD Are Victims of Child Abuse
This is not always the case.
While some cases of borderline personality disorder stem from childhood trauma, a diagnosis is more likely to be the result of a combination of environmental factors. These can include attachment, childhood trauma, biological factors, and social factors.
The Myth of BPD and Gender
Once more commonly diagnosed in women, the largest study done on psychiatric disorders shows that it occurs equally often in women and men.
One explanation behind it appearing to affect more women is that women are more likely to seek mental health care than men. Since research on BPD is often conducted in psychiatric settings, it was previously less likely for men with borderline personality disorder to be included in these research efforts.
Another explanation is that BPD is often misdiagnosed in men. Many men with the condition are often diagnosed with depression or PTSD.
Or perhaps the issue is that for years, the general public and many in the psychiatric community have viewed mental illness in boys and mental illness in girls in very different ways.
The Bias of Behavior
To illustrate this gender bias, psychologist Alan E. Fruzzetti, PhD, offers a simple test.
“If I told you that a student in a classroom was pounding on a desk and being disruptive, would the image of a boy or a girl enter your mind?” he asks. “Or, if I told you that a student in a classroom was upset and incessantly tapping on a desk, would you think it was a boy or a girl?”
Most of us would imagine the “pounding” student was a boy and the “tapping” student was a girl. And, when observing essentially the same behaviors, many people would describe them and react to them very differently, according to the gender of the person displaying the behavior.
There are various factors as to why we view boys and girls through different lenses.
Different behaviors are deemed acceptable or troubling depending on one’s gender, leading to different social responses for boys and girls.
In general, a girl who is angry, depressed, or displaying other signs of distress has a better chance of being treated with compassion and understanding—and being referred to counseling and treatment—than a boy.
In contrast, boys who show similar behaviors are often punished or ignored completely.
“The problem is that both boys and girls display ‘non-normative’ behaviors, and our misunderstanding of these behaviors has produced serious consequences for their mental health,” Fruzzetti explains.
Gender Gap in BPD Diagnosis
This gap between boys and girls is particularly present in the diagnosis and treatment of BPD.
BPD affects approximately the same number of men and women, but the condition is likely slightly over-diagnosed in women and significantly under-diagnosed in men.
Many studies have explored the differences between men and women who meet the criteria for BPD, finding that more men with substance use disorders are diagnosed with BPD than women, while more females with eating disorders or PTSD are diagnosed with BPD.
“When boys don’t fit social and emotional norms, their behavior can be misinterpreted,” Fruzzetti says. “Bias around gender may have a lot to do with these different diagnoses.”
For example, when men display anger, it is more often seen as a sign of antisocial behavior than it is in women, even though women with BPD show more aggression than non-BPD women, and men with BPD show less aggression than non-BPD men.
Also, established stereotypes about the nature of masculinity can lead to BPD being misdiagnosed or missed altogether.
Fruzzetti states that boys generally possess fewer social and emotional skills compared to girls, which is often misunderstood and incorrectly attributed to a lack of motivation or flaws in character.
Challenges of BPD in Boys and Men
Because of misdiagnosis and underdiagnosis, many boys with BPD do not receive any treatment, receive the wrong treatment, or worse, end up in prison.
About 20% of males in the criminal justice system actually have BPD.
According to Fruzzetti, overall, our health care system is not set up to help men with BPD. In particular, the prison system does not provide proper treatment.
In prison, biases and stigma about mental illness are intensified. Boys and men who struggle with BPD are more likely to be punished rather than treated.
“The solution isn’t to be less compassionate towards women; it’s to be more compassionate towards men,” Fruzzetti says.
Recognizing Borderline Personality Disorder in Yourself—or Others
People with borderline personality disorder struggle with self-regulation. Self-regulation is the ability to manage emotions, thoughts, and behaviors in ways that have positive outcomes, like self-esteem and good relationships.
To be officially diagnosed, a person has to exhibit five or more related symptoms. These symptoms have to be ongoing and impact various aspects of life.
There are a handful of medically recognized symptoms of borderline personality disorder.
Instability in Relationships
Intense and short-lived relationships are common for people with BPD. It’s very common for someone with this disorder to have intense, unstable relationships filled with drastic and quick-changing feelings.
A person with BPD may fall in love quickly and assume that the other person will make them happy. Typically, this results in the person feeling hurt and disappointed and can further intensify emotional swings. People with this condition may have either perfect or horrible relationships, with rapid changes in perception resulting from anger, hate, and devaluation.
Extreme Emotional Swings
Someone with this condition often experiences unstable moods and emotions. The little things that don’t mean much to others—like someone not holding the door open for you or meeting a new friend—can be either very exciting or frustrating.
Many with this condition can be happy one moment and extremely sad or disappointed the next. Their moods are also very intense and unpredictable in timing. They can last anywhere from a few minutes to a few hours or longer.
Explosive Feelings of Anger
Many people with BPD struggle with intense anger and a short temper. This makes it difficult for them to feel in control of their emotions once they have been provoked. They can quickly fill with rage, though this anger may not always be outwardly directed and can result in self-harm. Sometimes the person might be angry at themselves and not at anyone or anything else.
Self-Harm
Self-harm is risky behavior that may make the person feel good at the moment of distress. Many people with BPD often engage in self-harming activities, think about suicide, and make suicidal gestures and threats.
Many people with borderline personality disorder engage in sensation-seeking behavior that could be harmful, especially when they are angry.
Risky or deliberate self-harm activities may include:
- Engaging in dangerous and unhealthy binge drinking
- Cutting or other self-injury
- Going on shopping and spending sprees
- Regularly engaging in unsafe sex
- Using drugs
Not all self-harm is intended to end in death. It’s important to remember that it’s often used as a way to feel better in a grim moment. However, if it goes untreated, these risky behaviors can end in suicide.
McLean’s Michael Hollander, PhD, an expert in self-harm in adolescents, helps us understand more about teen cutting and self-injury.
Lingering Feelings of Emptiness or Worthlessness
A lot of people with the condition struggle with emptiness or worthlessness. Many with BPD report feeling like there is a void inside of them or like they don’t matter. As a result, they often turn to sex, drugs, or food to try to feel satisfied.
Feeling Out of Touch With Reality
Many diagnosed with BPD feel suspicious about events in their lives. They struggle with feelings of suspicion and paranoia about the intentions of people around them. When they are stressed, they may lose touch with reality and become disassociated. Disassociation feels like being spaced out, foggy, or as if you exist outside of your own body.
BPD can be confused with other forms of mental illness, so a diagnosis is important. If you or someone close to you often has feelings of emptiness, loneliness, or insecurity that cause irrationality or impulsivity, it’s important to talk to your health care provider.
When Is It Time To See a Professional?
If you are experiencing any of the previously mentioned signs and symptoms associated with borderline personality disorder, please consult a mental health professional. This condition is common and treatable.
You should see a doctor any time your symptoms are triggered. If you are unsure of your triggers, try to think of a time in the past when you experienced raging and intense emotions, acted impulsively, or had a desire to harm yourself. The events before this emotion are likely your triggers.
Many who have BPD experience suicidal thoughts. These can include but aren’t limited to mental images and fantasies about self-harm and plotting suicide. If you are experiencing suicidal thoughts and may harm yourself or someone else, call 911 immediately or visit your nearest emergency room.
Understanding and Recognizing Symptoms
People with BPD are sensitive to stress, so stressful situations activate symptoms related to the condition. The stressors that promote BPD’s most volatile symptoms can be external or internal, and they often vary from one person to another. There are both interpersonal and mental triggers of borderline personality disorder, many of which are unique to the individual.
Managing these symptoms, either for yourself or your partner, starts by understanding emotions, thoughts, and memories that set off symptoms. Then you can better manage addressing the symptoms if a stressor is unavoidable. You should work with a mental health professional to learn physical and mental exercises to understand triggers and develop skills to successfully manage them.
Interpersonal Relationship Events
Separations, disagreements, and rejections—real or perceived—are the most common triggers for symptoms. A person with BPD is highly sensitive to abandonment and being alone, which brings about intense feelings of anger, fear, suicidal thoughts and self-harm, and very impulsive decisions.
When something happens in a relationship that makes them feel abandoned, criticized, or rejected, their symptoms are expressed. People with borderline personality disorder experience rejection sensitivity, which makes relationships very intense and dependent. Events that can worsen this can be losing a job, ending a relationship, or experiencing rejection of any type.
Identifying Episodes
To better manage triggers, it is crucial to understand episodes. These episodes are highly dependent on the situation at hand and the specific individual, but there are common red flags for recognizing an episode.
Things that can indicate an episode is occurring:
- Intense angry outbursts
- Suicidal thoughts and self-harm behavior
- Going to great lengths to feel something, then becoming increasingly avoidant and withdrawn
- Paranoia, feeling as if there is someone out to get you
These episodes can also involve extreme feelings of positivity and euphoria. People with this condition can be very impulsive. It’s important to note these emotional highs as signs of an episode because they may be involved in risky behavior as well.
reating Borderline Personality Disorder
Treatment involves breaking down the dysfunctional patterns of the brain’s thinking, feeling, and behavior that cause distress to maintain a better emotional balance. Sometimes health care providers may suggest medication as part of a care plan.
The treatment options often used are general psychiatric management (GPM), dialectical behavior therapy (DBT), mentalization-based treatment (MBT), and transference-focused psychotherapy (TFP).
General Psychiatric Management
Sometimes referred to as good psychiatric management, GPM is designed to provide “good enough” treatment to most patients. This treatment is not inferior to others. Studies have shown that GPM can be as effective as DBT in treating patients.
GPM combines the essential ingredients of other treatments to provide care to the patient, even when specialized or more resource-intensive treatments are not available.
Dialectical Behavior Therapy
DBT is known as the gold standard BPD treatment. It emphasizes the development of four skill sets: mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance. DBT teaches patients to control their intense emotions and minimize their destructive patterns.
Through DBT, patients can also learn how to build interpersonal skills and develop self-awareness.
DBT has been clinically tested, proven to be effective in borderline personality disorder and depression treatment in adolescents and adults, and is used extensively at McLean Hospital.
Mentalization-Based Treatment
MBT aims to help patients by improving interpersonal and relationship skills while reducing self-destructive behaviors. Mentalizing focuses on the ability to differentiate and concentrate on your emotional state of mind and separate your own thoughts and feelings from those around you.
Since individuals with BPD can find it difficult to recognize the impacts of their behaviors, MBT encourages focusing and reflecting on mental states to better understand how mental state affects behavior in ourselves and others.
Transference-Focused Psychotherapy
TFP focuses on the patient’s sense of identity and aims to create more stable and realistic experiences of both self and others. With BPD, one’s sense of identity may feel contradicted. TFP focuses on addressing identity-based problems with interpersonal relationships, self-esteem, and mood.
By helping patients learn to verbalize what they are feeling—versus acting impulsively on emotions—TFP helps with increased functioning and satisfaction in interpersonal relationships.
In addition to these therapies, group and individual therapy may be useful as well. Group and individual therapies cover a broad range of topics and are not necessarily sessions dedicated to BPD. Group and individual therapy can be beneficial for addressing mindfulness, interpersonal relationships, stress management, emotion regulation, and family relationships.
How Is Borderline Personality Disorder Diagnosed?
Borderline personality disorder is a complex condition that doesn’t present itself the same way in every person.
Some mental and psychological disorders have similar symptoms, so it’s vital to see a licensed mental health professional for an assessment and the right diagnosis.
To diagnose, your provider may go through the following:
- A detailed interview with your doctor, a mental health provider, or both
- A psychological evaluation
- Medical history and/or a medical exam
- Discussing signs and symptoms, including criteria in the hallmark signs of BPD
Most diagnoses are in patients 18 and older. BPD can, however, be diagnosed in younger patients.
If you are experiencing the mentioned signs and symptoms associated with borderline personality disorder, please consult a mental health professional.
People with this condition often experience suicidal thoughts, such as mental images and fantasies about self-harm and plotting suicide. You should contact a suicide hotline number, a close loved one, or a mental health provider to get help.
Suicide prevention resources can be found below.
Good News: There’s Hope for Folks With BPD!
Because borderline personality disorder is as unique as each person who lives with it, treatment requires a specialized approach.
Many people have BPD and, at times, experience emotional anguish from the condition. However, you don’t have to resort to living a life that’s full of pain and heartbreak. It’s important to take care of yourself, recognize your triggers, and work with your health care team to determine what treatments will help keep it in check.
By committing to care and learning as much as possible about it, you can make a difference in your quality of life—and the lives of those around you.
Suicide Prevention Resources
Although it is not possible to predict suicide with any certainty, our best tool is recognition of the signs that many people exhibit when contemplating suicide. The following three behaviors should prompt you to seek immediate help for yourself or a loved one:
- Talking about wanting to die or to harm oneself
- Looking for a way to hurt oneself, such as searching online or obtaining a gun
- Talking about feeling hopeless or having no reason to live
If You or Someone You Know Needs Help
- Call 988 for the 988 Suicide & Crisis Lifeline
- Text HELLO to 741-741 for free, 24-hour support from the Crisis Text Line
- Outside of the U.S., visit the International Association for Suicide Prevention for a database of resources
- Contact your mental health professional
- Call us at McLean at 617.855.3141 for information on admission
Find more suicide prevention resources.
These organizations also offer suicide prevention resources:
988 Suicide & Crisis Lifeline
If you are suicidal, please call 988 or 800.273.TALK (8255). You’ll be connected to a skilled, trained counselor at a crisis center in your area. Counselors are available 24 hours a day, seven days a week. The 988 Suicide & Crisis Lifeline website also offers many resources for those looking for support.
American Foundation for Suicide Prevention
The American Foundation for Suicide Prevention (AFSP) is dedicated to saving lives and bringing hope to those affected by suicide. AFSP creates a culture that’s smart about mental health through education and community programs, develops suicide prevention through research and advocacy, and provides support for those affected by suicide. AFSP has local chapters in all 50 states, with programs and events nationwide.
Samaritans: Massachusetts 24-Hour Crisis HelpLine
A non-denominational, not-for-profit volunteer organization dedicated to reducing the incidence of suicide by befriending individuals in crisis and educating the community about effective prevention strategies. The Samaritans provide a free and confidential 24-hour phone befriending line. Call or text the 24/7 statewide Helpline at 877.870.4673.
Stop A Suicide Today!
Stop A Suicide Today is a nationwide campaign by Screening for Mental Health, Inc., to empower individuals to help themselves, colleagues, friends, and loved ones who are concerned about or feel suicidal.
Suicide Prevention Resource Center
The Suicide Prevention Resource Center is the only federally supported resource center devoted to advancing the implementation of the National Strategy for Suicide Prevention.
Comments
Post a Comment